Differences in Symptoms and Treatment Approaches between Thyroid Eye Disease in Children and Adults
Thyroid Eye Disease (TED), a common complication of Graves' disease, predominantly affects adult females and is characterised by swelling of the extraocular muscles leading to proptosis. A new study reveals that TED occurs in about 25 to 50% of patients with Graves' disease, with a higher prevalence among those with uncontrolled hyperthyroidism.
In the general population, the annual incidence of TED is approximately 3.3 per 100,000 women and 0.9 per 100,000 men, showing a clear female predominance. While specific sex distribution data in children versus adults with Graves' is not explicitly detailed, TED is generally more common in females, as Graves' disease itself is more prevalent in women.
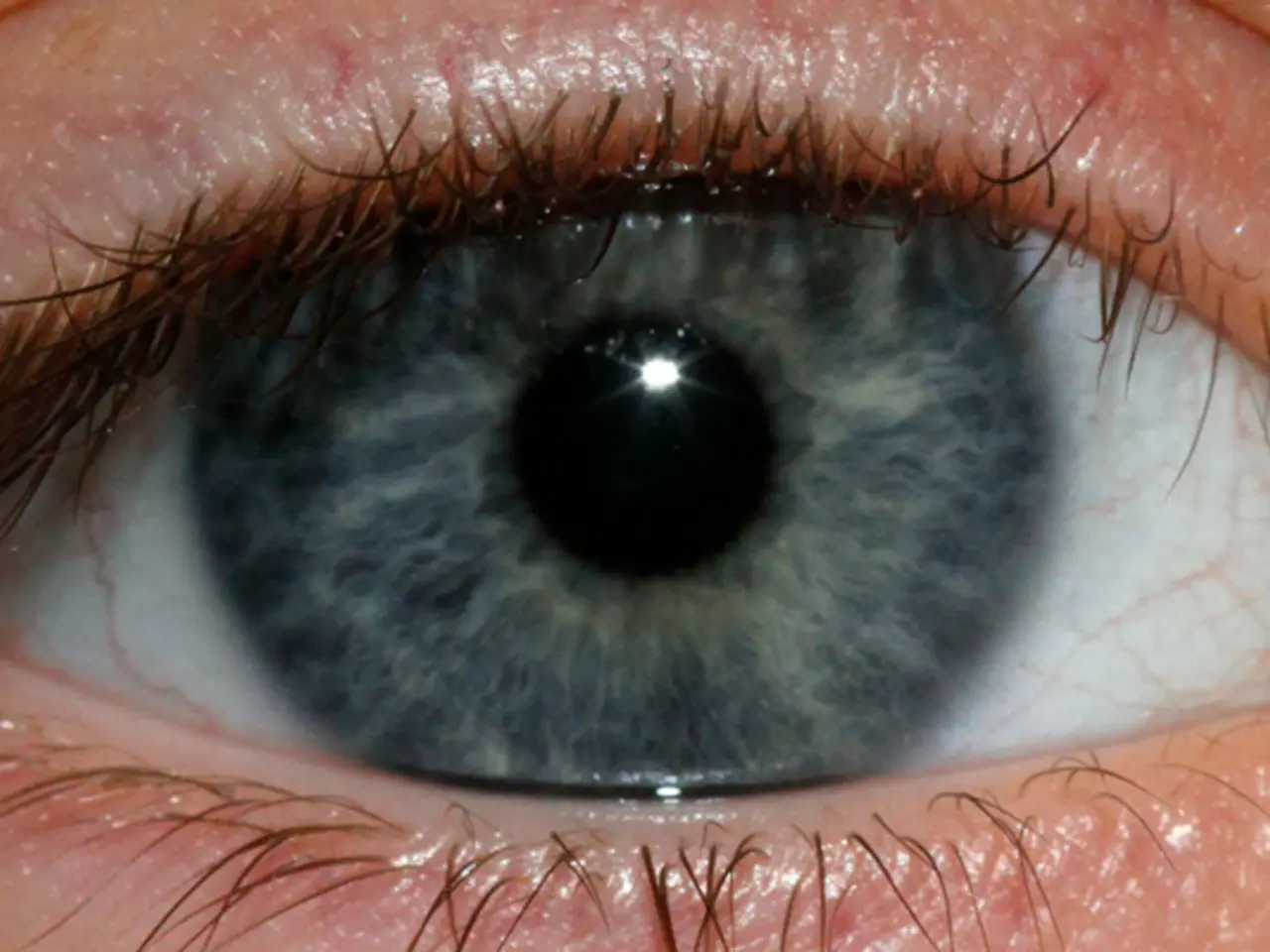
When it comes to clinical presentation, TED in adults typically presents with eyelid retraction, exophthalmos (proptosis), diplopia, orbital pain, eyelid swelling, and lagophthalmos, with potential serious complications such as vision impairment and dysthyroid optic neuropathy. On the other hand, pediatric TED is less well-characterized but is generally acknowledged in clinical literature that children often have milder clinical manifestations and lower rates of severe complications compared to adults.
The management of TED also differs between children and adults. In adults, treatment for active moderate to severe TED often starts with glucocorticoids, and if response is inadequate or intolerable, newer therapies like teprotumumab are indicated, especially within 9 months of steroid therapy. However, teprotumumab is approved for patients aged 18 years or older, indicating limited data or approval for pediatric use.
In children, management tends to be more conservative and focuses on controlling hyperthyroidism and monitoring for progression, with immunosuppressive or surgical interventions reserved for more severe or resistant cases. There is less evidence or approved medical therapy specifically for pediatric TED compared to adults.
Accurate assessment tools like the Clinical Activity Score (CAS), widely used in adults to gauge disease activity and guide treatment, may have limitations in reproducibility and subclinical detection, potentially complicating pediatric assessment as well.
In conclusion, TED is a common and potentially disabling complication of Graves' disease predominantly affecting adult females, with milder disease and less established treatment protocols in children. Adult management benefits from targeted biological therapies like teprotumumab, which currently lack formal pediatric approval. Careful clinical assessment is essential in both groups but may be complemented by specialized pediatric approaches in children.
Immunotherapy avenues with drugs like Teprotumumab can be explored for adolescents after their growth ceases. Clinical presentation of TED in adults includes redness, irritation, discomfort of the eyes and eyelids, retraction of eyelids, and exophthalmos or bulging of the eyes. Surgical risks in children demonstrate an inverse relationship with age, with higher complication rates observed in younger children.
Intravenous corticosteroids with weight-based dosing according to the Kahaly protocol are generally preferred for pediatric TED management. The natural course of thyroid eye disease in adults follows Rundle's curve, progressing through distinct phases: active (inflammatory) phase, peak phase, and chronic ("burnt-out") phase. In moderate to severe active TED in adults, an aggressive treatment plan for immunosuppression is required, including pulse therapy of intravenous corticosteroids.
In severe cases, it may lead to eye movement issues and diplopia. In juvenile Graves' disease, an estimated 33% to 67% of patients develop TED, with higher prevalence in teenagers (68.2%) than in younger children. In cases of hyperthyroidism in children under 5 years, thyroidectomy is performed.
TED affects both pediatric and adult populations. In adults, around 60% of Graves' disease patients are affected with TED, with peak incidence in the 40-49 and 60-69 age groups. Thyroid eye disease is an autoimmune disorder that can occur in patients with Graves' disease, Hashimoto's thyroiditis, or euthyroid individuals. Orbital radiotherapy targets activated orbital fibroblasts and inflammatory cells, reducing disease progression.
Females are more susceptible in paediatric cases, while adults show a bimodal sex distribution. In rare cases, orbital decompression or eyelid surgeries may be required for pediatric TED. Postoperative monitoring is crucial in children who have undergone thyroidectomy, particularly for potential complications such as hypocalcemia.
- The management of TED in children is more conservative, focusing on controlling hyperthyroidism and monitoring for progression, unlike adults who may benefit from targeted biological therapies like teprotumumab.
- Teprotumumab, despite its effectiveness in adult TED management, currently lacks formal pediatric approval for use.
- Intravenous corticosteroids with weight-based dosing according to the Kahaly protocol are generally preferred for pediatric TED management.
- The natural course of thyroid eye disease in adults follows Rundle's curve, progressing through distinct phases, while pediatric presentation is less well-characterized but often milder.
- Clinical presentation of TED in adults includes redness, irritation, discomfort of the eyes and eyelids, retraction of eyelids, and exophthalmos or bulging of the eyes.
- In severe cases of TED, both children and adults can experience eye movement issues and diplopia.
- Orbital radiotherapy, which targets activated orbital fibroblasts and inflammatory cells, is used to reduce disease progression in TED patients.
- In rare pediatric cases, orbital decompression or eyelid surgeries may be necessary due to the severity of TED.
- Postoperative monitoring is crucial in children who have undergone thyroidectomy to account for potential complications such as hypocalcemia.
- Thyroid eye disease is an autoimmune disorder that can occur in patients with Graves' disease, Hashimoto's thyroiditis, or euthyroid individuals, affecting both adult and pediatric populations.